News
Golfers on the Front Lines
Six essential workers from the New York City area share personal accounts of the pandemic and how golf is helping them cope.

Story and photographs by Alan P. Pittman
Through the years we’ve written extensively about the healing power of golf, from the ash-covered firefighters of September 11 who found a sense of peace and community in the game to the transformative stories of our Golf Saved My Life series. In moments of personal crisis, golf and fresh air can be profoundly cathartic. This seems to be as true as ever during the coronavirus pandemic. With the U.S. Open being played just outside New York City, the original epicenter of the virus in the United States, we invited six essential workers from the region who are golfers to share what it was like during “the surge” in March and April when the virus ravaged this city, killing more than 20,000 and overwhelming hospitals. What has it meant for these professionals to risk their lives to help others? How has golf helped them subsist? The virus has been in retreat here, but it continues to devastate large swathes of the country. More than 180,000 have died. These stories are a vivid reminder of the human cost, but also of our resolve and shared humanity.
HALEY CAMPBELL

• 25
• REGISTERED NURSE
• MORRISTOWN (N.J.) MEDICAL CENTER
• PLAYS AT WEEKAPAUG GOLF CLUB, WESTERLY, R.I.
My first day working in our COVID unit had the feeling of a science-fiction movie. It was shocking and disorienting. The symptoms of the patients coming in were severe and getting worse. A lot of them had to be intubated and, tragically, many of them didn’t make it. I remember thinking, Is this really happening? What is this virus? I can’t believe it can do this. But it was happening, and all of us had to adjust to the reality quickly.
For the patients I saw, I was primarily their only human contact. The doctors would come into the room if the patient really needed a full assessment, but otherwise I was it. I mopped the floors, took out the trash. I learned to draw blood. I did whatever needed to be done. I took a PPE [personal protective equipment] class to learn how to put on my protective wear. Before entering each patient’s room, I had to slip on a fresh pair of Crocs, gown up in surgical scrubs, put on an N95 respiratory mask and face shield and cover my hair as much as possible. It was hard because you’re sweating and rushing to get everything done that you need to. This was my routine for the 12-hour shifts I worked.
You get to know patients. You talk, you listen. They’re alone, sick and scared. Relatives weren’t allowed in the rooms, so I did my best to offer comfort. The Morristown community donated iPads so families could at least video chat. You had mothers telling their children through a screen not to worry. A husband reassuring his wife that he’d be fine. In many cases, family members would call the room even though the patient wasn’t responsive. They just wanted to say they loved them. It was gut-wrenching. During March and April, when things were bad, we had about 300 COVID patients in the hospital. It’s hard to describe how intense it was. As a nurse for only three years, I grew up fast.
There were low moments, like when a member of our hospital family passed away from the virus. And then the father of a close friend of mine was admitted with COVID, and I was assigned to be his nurse. I want to give all my patients the best care possible, but that one was personal. Thankfully, he survived, and just recently, a Facebook post of him at home with his family crossed my feed and made me smile. I was quarantined during this time in my apartment near the hospital. I couldn’t see my parents, who live a few hours north in Rhode Island, for much of the spring. I finally got a week off in July for my sister’s wedding. One of the first things I did was play a round of golf with my father. He’s a member of this nine-hole course on the water called Weekapaug. I used to work there during the summer and have played it many times. But on this day, with my dad, it was more special than usual. We talked, laughed and happily chased our balls, and, finally, for the first time in almost five months, I managed to take a deep breath and exhale.
SCOTT RUSSELL

• 54
• PARAMEDIC
• NASSAU COUNTY (N.Y.) POLICE DEPARTMENT
• PLAYS AT LIDO GOLF COURSE, LIDO BEACH, N.Y.
I’ve been a paramedic for 26 years, but this is my last. I’m retiring, thank God. The pandemic burned me out. During the surge here in the spring, I worked 800 hours in overtime. That’s like doing two shifts every day. One especially hard week I worked 16 hours each day for seven straight days. That almost killed me. It was all pandemic related. One call after another. Before the pandemic, I might get three emergency calls a day, but during COVID I averaged 14. And the calls were all the same: fever, cough, difficulty breathing. I didn’t need to see the test results. You know immediately that they have it. But what can I do? I have to take care of this person. I put the mask on and glove up. I know how transmittable this virus is. You say to yourself, Well, I could get this. I could get this today. What if he sneezes? What if my mask isn’t on right? I don’t know how I didn’t get it, but I didn’t. So I’m thankful.
We had six to eight of our paramedics test positive out of about 150. One was really bad. He was on a respirator, but he’s OK now. Things have finally calmed down. I might get one COVID call a week. Because of the nature of the job, you don’t really make connections with patients.
We rush them to the hospital and leave for the next call. During one drop-off, though, I looked up to see a nurse wheeling this elderly lady out. She must have been in her 80s, but she had beaten the virus. Everyone had lined the hallways and were clapping and cheering. It was a neat moment and a good reminder of why I’ve been in this job so long.
Reflecting on my career, one of my best days as a paramedic was when I was assigned to work the 2002 U.S. Open at Bethpage Black. I had access to areas regular fans didn’t. It was incredible. It was awesome. I cannot tell you. We had to be up early. I was there at 5:30, and throughout the whole day, I wasn’t even tired. I was on adrenaline.
What am I going to do now? Play more golf, I hope. I have a place in Myrtle Beach where my friends and I stay and play. We try to get down there once a month. Golf has always been my savior, and for years I’ve had this routine that sustains me. Literally next door to where I drop off my ambulance every evening is Lido Golf Course on the south shore of Long Island. Right on the water. I almost always go over there and hit some chips and putt a little. And when I do, all the stress from that day fades from my body.
CALVIN GARDNER
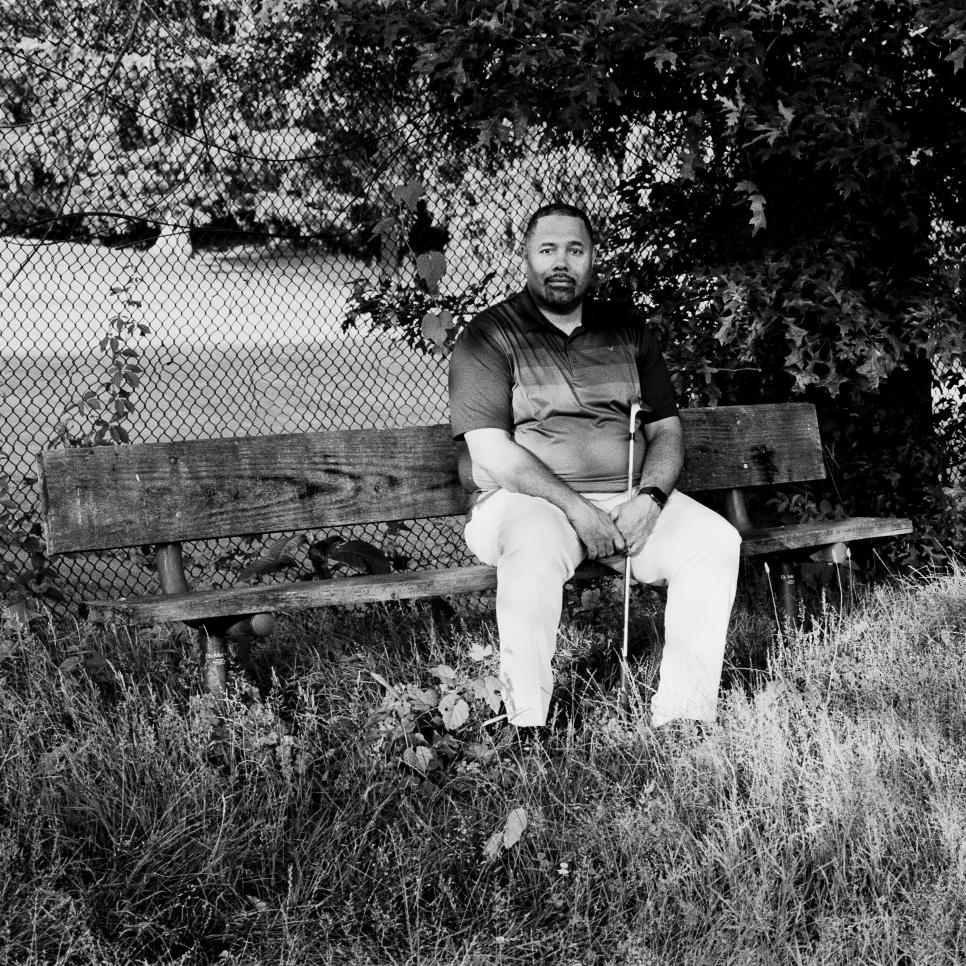
• 46
• SERVICE LINE DIRECTOR, NEUROSCIENCES
• STAMFORD (CONN.) HOSPITAL
• PLAYS AT E. GAYNOR BRENNAN MUNICIPAL GOLF COURSE
On April 29, I woke up earlier than usual, about 4 a.m., with an uneasy feeling. We were two months into the pandemic at the hospital where I work, but at that moment my thoughts were with my dad, who was an hour away at a different New York City-area hospital fighting for his life. He had gone to the emergency room on April 12 with allergy-like symptoms that turned out to be COVID. I called the hospital, and the nurse said my father had had a difficult night. I said I’d try to organize a FaceTime with our family, but 30 minutes later she called back to say my dad had passed. She said if I could get there within an hour, she’d let me see him. So I did, and I had just enough time to say a prayer, tell him I loved him, collect his things and leave. My father was 64, in good health and still active as a drummer in a band that played Motown-style music.
As an employee at a hospital near the original epicenter in this country and as someone whose family has been hit particularly hard by the virus—I’ve also lost two uncles, including one on my mother’s side—I’ve had an up-close view of its devastation. I’ve been heartbroken by what it has done to families but inspired by the empathy and resourcefulness of our hospital’s employees and surrounding community. It’s been an all-hands-on-deck type of mentality. My role changed entirely when the pandemic hit, as it did for many of my colleagues. I’m an administrative executive on the neurosciences team, but during COVID I’ve been managing 40 of our people who screen all employees coming into the hospital.
We do temperature checks, ensure everyone has a mask on, assess anyone with questionable symptoms and do contact tracing of anyone who tests positive. To date we’ve conducted more than 150,000 screenings. In the process we identified more than 100 people that we had to send home, some of which tested positive for COVID, so we believe our efforts have kept our work environment safe. Another important decision we made was to assign a staff member to each COVID patient in the hospital. The main job of that person was to communicate with the family, provide daily updates and facilitate video chats.
This was something that was personal to me. During the two and a half weeks my dad was in the hospital, it was difficult to schedule video talks. The hospital didn’t have the staffing. Let me just say that nobody should die alone in a hospital room unable to see their loved ones.
I’ve been in health care for almost 25 years. It’s my calling, but the pandemic has tested my limits physically and emotionally. I’m thankful to have two wonderful daughters, family and friends for support, and I’m grateful to have golf. It’s been a weekly part of my life since I took it up 10 years ago. The serenity of being outside with friends is my stress-reliever.
I really missed it during the lockdown. But I’m back out there now, finding peace, catching up with old friends and making new ones.
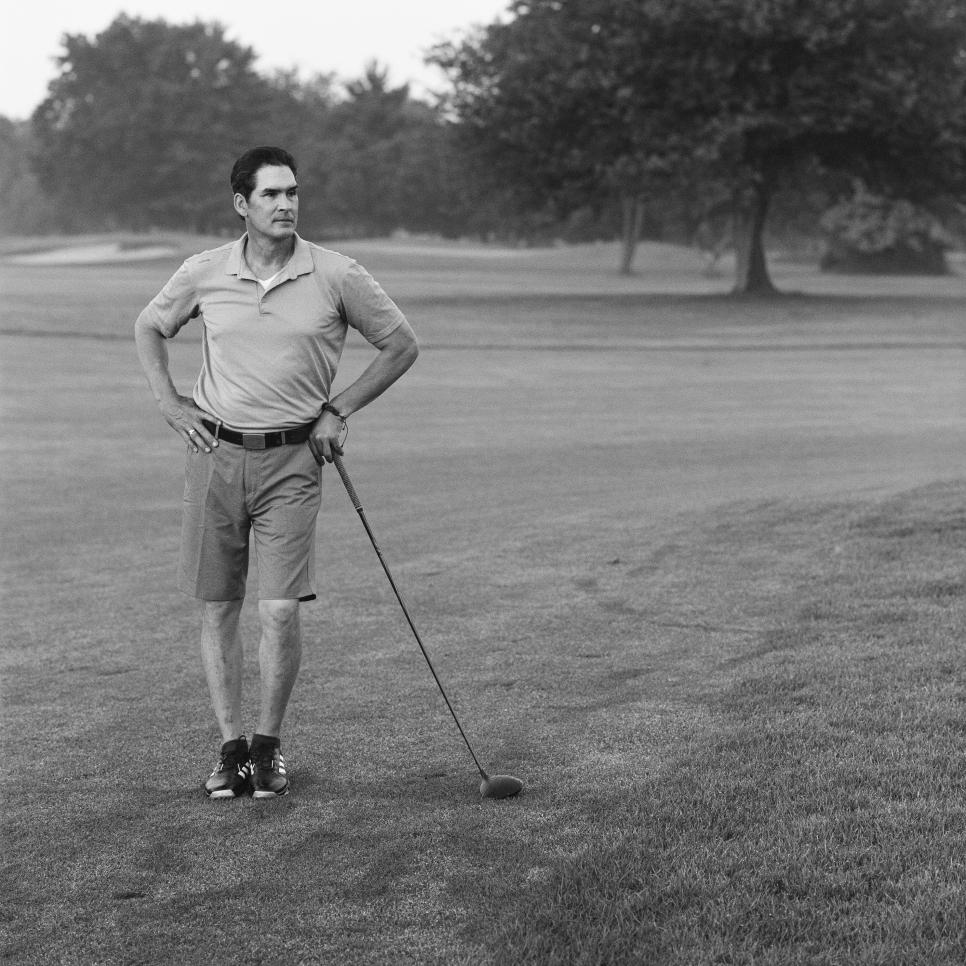
STEVEN TEPPER

• 51
• DEPUTY CHIEF, CUSTOMS AND BORDER PROTECTION JOHN F. KENNEDY INTERNATIONAL AIRPORT
• QUEENS, N.Y.
• PLAYS AT BETHPAGE BLACK
I love being a U.S. Customs and Border Protections officer. What I do every day means something, and no two days are alike. Last year we processed more than 17.2 million international passengers, conducted thousands of counterterrorism searches and seized millions of dollars in illegal narcotics. The job has it all. The virus, however, has been a challenge unlike any other.
I was actually on a golf course in Florida for a buddies trip in early March when my boss called to tell me I would be helping head up the airport’s Coronavirus Command Center. In many respects we were well prepared. We had all the personal protective equipment we needed and had begun to put in place safety protocols and best practices developed by our health and safety team. Because of a drop in airline traffic we were able to place those with underlying health conditions or other critical factors on administrative leave. But when you have 1,200 officers and thousands of people streaming in from around the world every day, it’s unrealistic to think people aren’t going to get sick.
My job was to check in daily with anyone who became ill. If they tested positive, my team performed contact tracing going back 14 days and quarantined anyone who interacted with them. Despite our best efforts, officers have died. One of them was a really close friend of mine. We started working at the airport at the same time, in 2003, went through training together, spent our first year on the job together. He was only 40 and such a tough kid—much stronger than I am. But the virus hit him hard and fast. He was on a ventilator for a month before he passed away.
I tell everybody it’s not just a fever and cough. One guy had the sniffles. Another couldn’t breathe. Yet another had nothing. So the symptoms run the gamut. And you can be tough, young and healthy like my friend. The virus doesn’t care. That’s why it’s important to avoid non-essential travel right now. And if you have to travel, make sure to wear a mask and follow CDC guidelines to protect us as well as yourself.
Among employees, there’s certainly apprehension about being on the front lines, but also a sense of duty and pride in our work. We’re New Yorkers. Things have slowly returned to normal at the airport, and we’ve become smarter and more efficient at protecting our people.
I’m on a schedule where I work seven straight days before getting time off, and the only way I get through the week is to know on the eighth day I have a tee time with my buddies. The course is where I get to take off the shield and enjoy some fresh air and exercise. I belong to the Nassau [County] Players Club. It’s a golf league that plays out of Bethpage Black made up of a lot of New York City cops, firemen and other first responders. Golf and the camaraderie are our therapy. And right now, we need it more than ever.
NOEL O’CONNELL
• 57
• CONDUCTOR, LONG ISLAND RAIL ROAD
• PLAYS AT EISENHOWER PARK GOLF COURSE, EAST MEADOW, N.Y.
As the conductor, I’m in charge of the train. I work with an engineer and a brakeman to get people from Point A to Point B. During the pandemic I’ve been transporting essential workers only—hospital staff, police officers, fire fighters, paramedics and the like—back and forth from Babylon, N.Y., to Penn Station in Manhattan. The trip takes about an hour and a half one way with 17 stops, and I make the round trip twice in a day. I’d like to say it’s only front-line workers I see, but I also have to deal with drunks, folks trying to hop a free ride or not wanting to wear a mask. They sit next to these exhausted nurses, and I have to come out of my cab with my mask and gloves on and try to reason with them. Too often they get belligerent, irate, and I have to radio the cops and hope they show up four stops down the line and remove them. It’s unfortunate. It endangers lives, and I have to be careful how much I engage them. My 83-year-old mother lives with me and my girlfriend and her son. The last thing I need is to bring the virus home—a sentiment you hear a lot from essential workers.
I’ve had one close call that I know of. I played golf with another conductor, a good friend of mine, and a couple days later he tested positive. I got tested, and it came back inconclusive, which is unusual, I was told. They had to treat me like I was positive, so I self-quarantined for two and a half weeks. Thank God I never showed any symptoms. Several of our people working the trains have tested positive. I just don’t know how you avoid it.
On my route each day I see many of the same faces and have gotten to know some of them. I’m in awe of what they do, honestly. I see them after crazy-long shifts. They’re drained, and they’ve had to deal with a lot of bad stuff. Many of my friends are police officers. When I see some of them at Penn Station, especially the ones working down in the subways, the atmosphere is thick. It’s mostly, “How are you doing?” and “Stay safe, my friend.”
For the ones that ride my train, I wanted to do something, so I added a personal note to the regular announcements: I want to take this time to thank all you essential workers out there for all the hard work and all the things you do for us. My crew and I are grateful. It’s a small gesture, but I was surprised by how many people stopped me to say thank you for that. We all need to feel appreciated. Between all the nonsense in this job, I do get to meet some good people.
It’s nice. Relationships are important in this life. That’s one of the beautiful things about golf, right? The friendships you make. I spend the majority of my hours at work walking back and forth in a metal tube, dealing with people and situations I can’t always control. I need an escape that’s familiar and comforting, and when I’m on the golf course, I know what I’m getting: I see smiles. I see love. I see hope.
ROD ACOSTA

• 62
• CHIEF PHYSICIAN EXECUTIVE, STAMFORD HEALTH
• PLAYS AT INNIS ARDEN GOLF CLUB, OLD GREENWICH, CONN.
I’ve been a family-medicine physician for 33 years, and I still see patients, including ones with COVID-19, but in my role as CEO of Stamford Health Medical Group, which consists of 200 physicians, I’ve been helping manage our response to the pandemic.
When we first began seeing waves of patients—25, 30 admissions a night with COVID—we weren’t sure if we’d have enough PPE and staffing to care for them. At one point we had 150 COVID-19 patients in the hospital, 44 of them intubated, when our average is just four patients on ventilators. It was scary. We were burning through 3,500 gowns, 357 N95 masks and 1,400 surgical masks a day before implementing a rationing policy. Our cost for PPE (masks, gowns, gloves and face shields) jumped from $125,000 a month to $640,000.
When I think about those weeks, what stands out are the stories that reveal the best of ourselves. We had a young woman from Guatemala who was seeking asylum. She came to the hospital pregnant and very sick with COVID.
It required our ICU and Labor and Delivery teams to coordinate. If her condition deteriorated, she would need to be intubated, and the baby would have to be delivered before she went on a vent. Sure enough, within 24 hours, she needed to be intubated, and we did the C-section right away. The baby was healthy, COVID-free. The mother remained in the ICU but eventually left the hospital and is doing very well. The baby’s father and his son also had COVID, so the baby didn’t go home right away. One of the son’s schoolteachers took care of the baby until the mother was well enough. You draw inspiration from good outcomes like these.
COVID’s impact on this Latino family wasn’t unique. We noticed early on that Latino and Black communities were experiencing COVID more severely than others. One reason is that their living situations tended to be more concentrated, and they were less able to practice social distancing. As a result, we launched a task force that coordinated with government agencies, health-care providers, food pantries, schools and organizations that support immigrants and vulnerable populations. PPE and educational resources were distributed to everyone living in subsidized multifamily housing units. There’s little doubt these measures saved lives.
We’re now down to fewer than five COVID-19 patients at any given time, and we made it through this with the resiliency and excellent care of our physicians, nursing staff, clinical staff and with the support we received from the community.
Golf has been my private Idaho. It takes my mind off other things like nothing I’ve ever tried. It’s the perfect sport for COVID. I play twice a week, walking and carrying my bag, and it’s easily when I’m most relaxed. My wife, Barb, and our two sons, Matthew and Lucas, are golfers, too, and a tradition of ours has been to play as a foursome on Sundays. It’s our family time.
I tend to be a very positive person—in my approach to patient care and golf. Perhaps that’s why I still play. I always think I have it in me.
• • •
MORE U.S. OPEN 2020 PREVIEW CONTENT FROM GOLF DIGEST: Every Hole at Winged Foot: Exclusive drone footage | Can you read a Winged Foot green? | 13 best bets for the 2020 U.S. Open | Ranking the top 100 players in the field at the 2020 U.S. Open | 8 interesting revelations about the epic 2006 Open at Winged Foot | The ‘other’ miscues that cost Phil Mickelson the 2006 U.S. Open | Interactive guide to New York’s great golf courses | A super-scientific ranking of Winged Foot’s 11 previous major championships | 7 shots that can make or break any round at Winged Foot | At Winged Foot, a pandemic stirs memories of the last time the world stopped | The Winged Foot mystique | The 15 best U.S. Opens, ranked | The return to Winged Foot means a return to this USGA favorite—gnarly rough | Our latest podcast sifts through Phil Mickelson's Winged Foot collapse to unearth lessons for the rest of us | I played Winged Foot from the championship tips on camera, and it was probably a bad idea

